Measuring human brain activity remains one of the biggest challenges in science and medicine. Despite recent technological advances in areas such as imaging and nanoscience, researchers still struggle to accurately detect cognition. Currently, functional magnetic resonance imaging (MRI) is used to measure brain activity, but this method requires the patient to lie quietly in a large, noisy and expensive device. A portable, non-invasive method is needed to elucidate how the brain functions in a more natural environment while performing activities of daily living.
In 2013, the National Institutes of Health launched an initiative to encourage more neuroscience research by funding projects in key areas of the field. One project, led by the Athinoula A. Martinos Center for Biomedical Imaging at Massachusetts General Hospital (MGH) in collaboration with MIT Lincoln Laboratory and Boston University, is developing a high-performance brain imaging method that can more accurately monitor brain blood. Stream more than ever. The brain regulates blood flow in different ways depending on the mental and physical tasks a person is performing. Using a portable system to accurately map cerebral blood flow will give researchers insights into cognition.
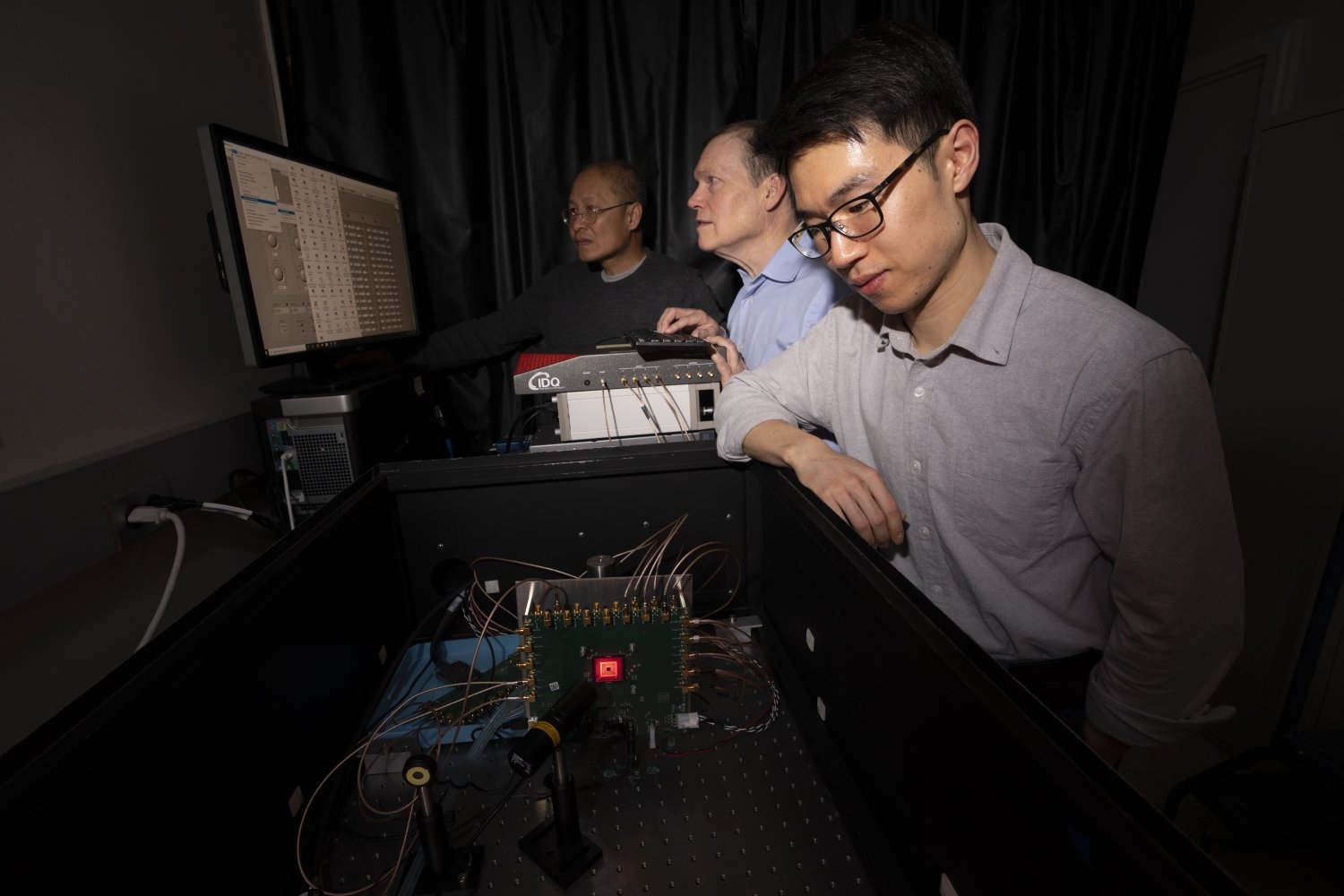
“This new method, called time-domain diffuse correlation spectroscopy (TD-DCS), works by using optical fibers to deliver laser light to and from the brain,” said research team member Jonathan Laboratory’s Advanced Imaging Technologies Group. Richardson said. The method will be integrated into a hat-like system with 64 transmission points and 192 reception points organized into groups called optodes spaced 1 centimeter apart and covering nearly the entire scalp. “Light diffuses from the emitter at each optode, bounces off the hemoglobin in the red blood cells, and then returns to several surrounding receivers.”
Blood cells are constantly moving, and the faster they move, the faster the intensity of the returning light signal fluctuates. Researchers can use fluctuation rates to measure blood flow velocity.
Early in the program, the team worked on optimizing the wavelength of light used for the pulses. Tissue and blood absorb and scatter light at different wavelengths differently. These effects can eat up light signals so that none of them are reflected back to the receiver. Through modeling and measurements, they determined that a 1,064-nanometer laser could safely deliver nearly 11 times more photons than the shorter wavelengths currently used and reach 25 percent deeper into the brain. In addition, commercial pulsed fiber laser technology can easily produce 1,064-nanometer lasers.
To make the receiver sensitive to the faint light signals returning from deep inside the brain, the team used a custom detector technology developed at Lincoln Laboratory called a Geiger-mode avalanche photodiode (GmAPD).
“A GmAPD is a device that emits rapid electrical pulses in response to a single photon,” said researcher Brian Aull. “We can detect this pulse and digitally measure when it occurs, which makes the detector very sensitive. We need this because most of the light is scattered in random directions and only a small amount is scattered in the correct direction to reach the detector.”
For two decades, these GmAPDs have been involved in many of Lincoln Laboratory’s key projects. This project is the first medical application of GmAPD, which is combined with a new readout integrated circuit (ROIC) designed specifically for this purpose.
“After years of development and demonstration for astronomy and national security applications, we are excited to see the impact our detector technology has on medicine,” said Erik Duerr, leader of the Advanced Imaging Technology Group.
GmAPD technology also solves the problem of irrelevant return light signals, particularly those that reflect from cells in the scalp rather than blood in the brain, which can confound results.
“They are gated,” Orr said, “which means they can only turn on during selected time intervals.” Photons bouncing off the scalp will return to the optode faster than photons coming from deep within the brain. “By using delayed turn-on, the system can ignore these early photons.”
So far, the team has successfully demonstrated TD-DCS at 1,064 nanometers in human subjects using a separate commercial detector. They are now focused on implementing and testing ROIC and GmAPD integrated detectors. In 2024, they plan to hand over the system to the MGH team, which will then integrate it with the laser system.
“This technology has direct clinical relevance to the diagnosis and tracking of traumatic brain injuries and can monitor brain perfusion during on-site trauma care,” Richardson said. “In the long term, we hope this technology can help treat psychiatric disorders.” Illnesses such as post-traumatic stress disorder, depression and suicidality in soldiers.”